Comparison of Weight Control Attempts among Middle-Aged and Older Women with Obesity: Findings Based on the Seventh Korea National Health and Nutrition Examination Survey (KNHANES VII-3)
Abstract
We compared weight control attempts in middle-aged and older women with obesity via a cross-sectional study of 1,571 women aged ≥ 50 years based on data from the Korea National Health and Nutrition Examination Survey. Among the participants, 57.7% were overweight or obese, and the obesity rate of participants in their 70s was the highest. While 71.7% of women had attempted to lose or maintain weight, the older age groups were less likely to attempt intentional weight control than the younger age groups. The prevalence of weight control attempts was significantly different amongst the age groups, with the lowest rate observed in the 70s group after adjusting for BMI, WC, and chronic diseases. In particular, 41% of participants in the 70s group with obesity did not attempt to manage their body weight. Among the participants who tried to maintain or lose weight, the most commonly practiced weight control strategy was reducing the size of meals. Compared to the 50s group, the 70s group was less likely to attempt weight control. While body image was the most significant indicator of weight control attempts in the 50s group, educational level was the key factor associated with weight control in the 70s group. Our findings reflect an active investment by older Korean women in body weight management and provide insight into policy efforts that may help women with obesity maintain a healthy body weight.
Keywords:
Diet, exercise, middle-aged women, older women, weight control, obesityIntroduction
Although significant efforts to maintain a healthy body weight have been undertaken worldwide, the prevalence of obesity has not decreased; in fact, it remains an urgent public health problem (World Health Organization, 2020). Meanwhile, as life expectancy worldwide consistently increases, Korea has become one of the world’s fastest-aging countries (Jang, Lee, Lee, & 50th Anniversary Committee of Korean Geriatrics, 2019). Evident changes in body composition with age include increased fat mass and decreased muscle mass, which lead to gradual weight gain (Westerterp, 2018). Substantial evidence has shown that obesity in older individuals increases cardiometabolic risk, physical disability, and impaired quality of life (Han, Tajar, & Lean, 2011). It should be noted that > 40% of older women have obesity, and the rate of female obesity increases with age, while that of male obesity decreases with age (Jang et al., 2019).
Older individuals with obesity should engage in weight control treatment involving structured lifestyle interventions with clear clinical goals including reduction in cardiovascular risk and improvements in mobility and physical function (Moredich & Kessler, 2014). This is despite the existing epidemiological reports that discuss an “obesity paradox” based on the results that lower mortality rates were observed in older people with obesity than in lean individuals (Dorner & Rieder, 2012). Weight loss inevitably reduces both fat and lean mass, exacerbating weakness and muscle dysfunction (Santos, Sniehotta, Marques, Carraca, & Teixeira, 2017; Weinheimer, Sands, & Campbell, 2010). Moreover, older patients are likely to have abnormalities in metabolic function, subclinical cardiovascular diseases (CVDs), and nutritional deficiencies, increasing the risks associated with various weight loss interventions (Moredich & Kessler, 2014). To help older women maintain a healthy body weight, an understanding of the weight control behaviors of women with obesity is required.
In the NHANES study, the proportion of elderly people (over 55 years old) who wanted to lose weight was similar to that seen in younger people (under 55 years old) (Yaemsiri, Slining, & Agarwal, 2011). However, whether older women try to maintain or lose weight remains unclear. A significant number of studies on weight loss efforts among adults exist, but studies including older age groups are limited (Faucher & Mobley, 2010). In particular, quantitative data on weight control attempts in older women are insufficient (Jang et al., 2019). Identifying differences in the personal weight control efforts of women with obesity by age is necessary to establish targeted obesity management protocols for older women.
We aimed to compare weight control attempts and methods used among community-dwelling women in their 50s, 60s, and 70s with obesity using a large-scale nationally representative dataset. We hypothesized that there would be differences in efforts to control body weight and factors associated with weight control attempts in women with obesity by age group. Our findings provide epidemiological data on current trends in weight control efforts among middle-aged and older women and help develop evidence-based, practical weight control strategies.
Material and Methods
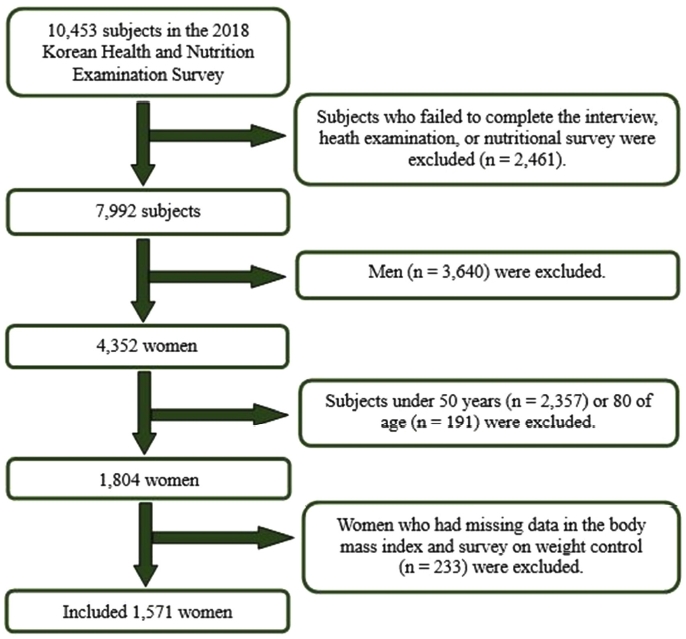
The data used in this study were collected from the 7th Korean National Health and Nutrition Examination Survey (KNHANES VII-3) in 2018. It includes a complex, stratified, multistage sample, and the results are open to the public. This study included women aged ≥ 50 years (Figure 1). Men (n=3,640), women under 50 years (n=2,357), or 80 years of age (n=191), and those who had missing data in BMI and survey on weight control (n=233) were excluded. Ultimately, 1,571 women were included in the statistical analysis. The KNHANES was approved by the Institutional Review Board (IRB) of the KCDC (IRB No:2018-01-03-P-A).
Clinical investigation
Trained interviewers and medical staff performed the interviews and health examinations. Current medical conditions were defined as those that were diagnosed and/or treated by a doctor. Hypertension (HTN) was identified through blood pressure measurement and an interview questionnaire, while diabetes mellitus (DM) and hyperlipidemia were identified through blood sample analysis in a fasting state and questionnaire. The self-administered questionnaire covered smoking status, alcohol use, activity limitations, and aerobic exercise. A current smoker was defined as one who had smoked cigarettes daily or on some days. A drinker was defined as an adult consuming at least one drink per month. Aerobic exercise was defined as performing moderate physical activity for ≥ 150 min or vigorous physical activity for ≥ 75 min per week (Piercy et al., 2018).
Anthropometric and laboratory measurements
Health examinations were conducted in a mobile examination center and included physical examinations and anthropometric measurements. Height and weight were measured to the nearest 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Results were classified based on BMI categories appropriate for Koreans: underweight (BMI < 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), and obese [Class I (25-30 kg/m2), Class II (30-35 kg/m2), and Class III (> 35 kg/m2)] (Seo, Lee, Kim, Kang, Kang, Kim, & Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity, 2019). Waist circumference (WC) was recorded midway between the lower margin of the final rib and upper margin of the iliac crest to the closest 0.1 cm. Abdominal obesity was defined as WC ≥ 85 cm or higher (Seo et al., 2019). The laboratory data quality control program monitored the laboratory performance to ensure that the data met the required standards of accuracy (Kweon et al., 2014).
Dietary intake
Trained interviewers performed computer-assisted personal interviews to assess dietary intake. A 24-hour recall dietary questionnaire based on typical Korean food items was used (Shim, Oh, & Kim, 2014). Its open-ended response structure allowed the respondents to provide a comprehensive and detailed report of all foods. Food models, pictures, and other visual aids were used to help respondents judge and describe the portion size and improve accuracy. All food products ingested by the study participants during the previous 24 hours, together with dietary information (time, location, type of food, amount, and cooking method), were investigated. The amount of total energy and nutrients consumed was calculated using a food composition table published by the Rural Development Administration of Korea, which has acceptable validity and reliability (Rural Development Administration, National Institute of Agricultural Sciences, 2018).
Questionnaire on weight control
Intentional weight control attempts were assessed by participant self-reports (or interviews for participants with low literacy) that involved the following questions and choices: “Have you tried to control your weight in the past year” ([1] to lose weight, [2] to maintain weight, [3] to gain weight, [4] never tried to control weight)?” Thereafter, participants who answered [1] or [2] to the above question were asked to choose what they did for weight control and were provided with multiple choices: (1) exercise, (2) fasting for more than 24 hours, (3) diet control, (4) skipping meals, (5) taking an unprescribed weight-loss drug, (6) taking a prescribed weight-loss drug, (7) taking oriental medicine, (8) taking health functional food, (9) one food diet, (10) etc. Body image perception and 1-year body weight changes were also assessed.
Statistical methods
Weighted complex sampling analysis was used for all data analyses. Generalized linear regression for continuous variables and the chi-square test for categorical variables were used to compare general characteristics between age groups. To identify the factors associated with weight control attempts, we performed a univariate logistic regression analysis in each age group. Based on the analysis, household income, education level, chronic diseases, and body image were significant factors. Thus, we performed a multiple logistic regression analysis to confirm whether household income, educational level, and self-perception of body image were still associated with weight control attempts after adjusting for age, BMI, WC, and chronic diseases. Additionally, to compare the odds ratio (OR) and 95% confidence interval (CI) of weight control attempts in the 60s or 70s group versus the 50s group, multiple logistic regression analysis of the complex sample was performed. Statistical analyses were performed using SPSS 23.0 (IBM Corp., Armonk, NY). In all analyses, P < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of the study subjects
A total of 1,571 women participated in the study (mean age, 62.1 years). Women in their 70s had a lower household income and educational level, higher rate of chronic diseases, were less likely to live with their spouse and consume alcohol and were less likely to be current smokers or be physically active than women in their 50s or 60s. In contrast, women in their 70s had significantly higher BMI and WC than those in their 50s or 60s. Regarding dietary intake, older women had lower intakes than younger women. However, the amount of carbohydrate intake did not differ across age groups (Table 1).
Obesity status of study participants
Figure 2A shows the obesity status of the participants. Approximately 57% of women were overweight or obese, and only 40.3% had normal body weight. The obesity rate was significantly higher in the 70s group than in the 60s or 50s groups. Approximately one-third of the total women were classified as having abdominal obesity (Figure 2 B). The 70s group had the highest abdominal obesity rate (46.5%). Compared with the 50s group, the 60s and 70s groups had a higher risk of abdominal obesity.
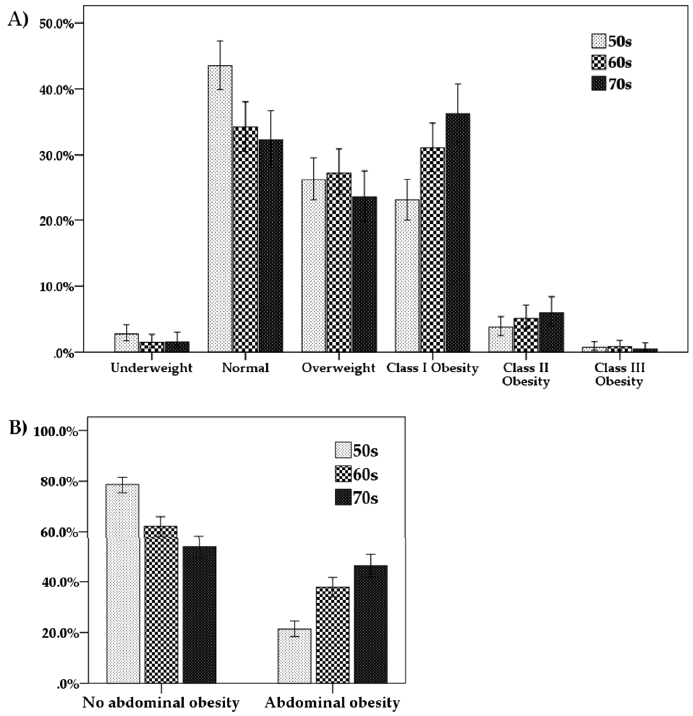
Distribution of obesity status defined based on body mass index (A) and waist circumference (B) by age groups. Underweight, body mass index < 18.5 kg/m2; normal, between 18.5 and 22.9 kg/m2; and overweight, between 23 and 24.9 kg/m2. Class I obesity, between 25 and 29.9 kg/m2; Class II obesity, between 30 and 34.9 kg/m2; and Class III obesity, ≥ 35 kg/m2. Abdominal obesity, waist circumference ≥ 85 cm
Characteristics of women with obesity by age group
Among women with obesity, the 70s group had a lower household income and educational level, a higher rate of chronic diseases, and was less likely to be physically active and live with their spouse than the 50s or 60s groups. The 70s group had lower dietary intake than the 50s or 60s groups; however, the amount of carbohydrate intake did not differ across the age groups (Table 2). Women with obesity (n=533) did not have higher intake levels of calories (p = 0.251), carbohydrates (p = 0.592), proteins (p = 0.152), and fats (p = 0.081) than overall women (n=1,571).
Weight control attempts in women with obesity according to the different age categories
Table 3 shows the attempts and methods used by obese women to intentionally control weight in the past year by age group. More than 14% of obese women did not consider themselves overweight or obese. More than 70% of the women answered that they had tried to reduce or maintain weight for the past year. However, the older age groups were less likely to attempt intentional weight control than the younger age groups. In particular, 41% of women with obesity in their 70s did not attempt to manage their body weight. Despite intentions for weight reduction, body weight remained unchanged during the previous year in most obese women.
Methods of maintaining or reducing weight in women with obesity according to age group
Among the women who tried to maintain or lose weight, reducing the amount of food was the most commonly practiced weight control strategy across all age groups, followed by exercise and skipping meals (Table 3). Dietary supplements and oriental herbal medicines were used more frequently for weight management in the 50s group than in the 60s and 70s groups. In contrast, anti-obesity medications prescribed by doctors were less frequently used for weight control than dietary supplements.
Factors associated with weight control attempts in women with obesity
Age, household income, education level, DM, hyperlipidemia, and self-perception of body image were factors significantly associated with weight control attempts in women with obesity (Table 4). However, each age group had different factors. For instance, in the 50s group, women with a lower household income, educational level, and hyperlipidemia were less likely to use weight control strategies than women with a higher household income and educational level, and without hyperlipidemia. Moreover, in the 70s group, women with obesity and a lower educational level, DM, or inappropriate self-body image were less likely to use weight control strategies than women with a higher educational level, no DM, or appropriate self-body image. In the multiple logistic regression analysis adjusted for age, BMI, WC, and chronic diseases, household income, educational level, and self-perception of body image were still significantly associated with weight control attempts in the 50s group. However, in the 70s group, only lower educational level remained a significant factor associated with weight control attempts (Table 5).
Comparison of the prevalence of weight control attempts among age groups
The 60s and 70s groups were less likely to try weight control than the 50s group after adjusting for age, BMI, and WC (Table 6). In the multiple logistic regression model, including the presence of chronic diseases, weight control attempts were significantly fewer in the 70s group than in the 50s group. However, after additional adjustments for household income, educational level, and body image, the difference between the age groups was insignificant.
Discussion
This study investigated the prevalence of weight control attempts and methods used during the past year among obese Korean women aged > 50 years using nationally representative data. The results of this study indicate that the majority of community-dwelling women with obesity aged ≥ 50 years are trying to manage their weight using various methods. However, the prevalence of weight control attempts was significantly different between the age groups, with the lowest rate observed in the 70s group after adjusting for BMI, WC, and chronic diseases. We also confirmed that educational level, household income, and self-perception of body image were closely associated with efforts to control weight among middle-aged and older women with obesity.
The literature on weight control attempts among older women based on a large-scale dataset representative of the general population is insufficient, as most previous studies have included young or middle-aged women (Faucher & Mobley, 2010; Williams et al., 2007). To our knowledge, this is the first study to present estimates of the prevalence of weight control attempts and methods used and describe the related factors among middle-aged and older Korean women. This is clinically important because accurate and reliable data in this area can assist in evaluating trends and changes in obesity worldwide, and in setting priorities for public health initiatives in aging individuals with obesity.
Increasing prevalence of obesity with age
The high rate of weight control attempts in our study subjects indicates national overweight and obesity trends. During the past 10 years, the obesity rate in South Korea has consistently increased, mostly in older women (obesity rate, > 40%) (Jang et al., 2019). Similarly, our study found that the obesity rate, defined based on BMI or WC, increased with age. Older individuals experience normal physiological alterations in body composition, such as increased total body fat (BF) content, decreased lean body mass (LBM), and more centrally distributed fat (Han et al., 2011).
Meanwhile, several recent studies have described an “obesity paradox,” where older adults with higher BMI are at lower risk of mortality from HTN, CVD, and Heart failure (HF) than their healthy weight counterparts (Dorner & Rieder, 2012; Flegal, Kit, Orpana, & Graubard, 2013). Multiple possible mechanisms proposed include a greater likelihood of receiving optimal medications due to earlier presentation of obesity; benefits of higher LBM, such as greater muscle mass, muscular strength, and higher metabolic reserves; and cardioprotective metabolic effects of BF (Chang, Asch, & Werner, 2010). Researchers have tried to explain this phenomenon by the lack of discriminatory power of BMI to differentiate between BF and LBM (Romero-Corral et al., 2006). However, others have demonstrated that even when using BF instead of BMI as the criterion for obesity, this association is consistently observed (Lavie, De Schutter, Patel, Artham, & Milani, 2011). Hence, fundamental questions remain (Flegal, Graubard, Williamson, & Gail, 2005; Flegal et al., 2013; Heiat, Vaccarino, & Krumholz, 2001). Nonetheless, obesity in older adults has a negative impact on functional status and quality of life (Apovian et al., 2002). Obesity is closely associated with physical weakness and slow movement (Lopez-Garcia et al., 2003). Therefore, clinical improvement with weight management in older adults should be clear, and physicians need to determine the risk–benefit profile of weight reduction before initiating obesity treatment. The importance of healthy weight should be emphasized to maintain LBM, muscular strength, and cardiorespiratory fitness.
High rate of weight control attempts that decrease with increasing age
The majority of obese women (71.7%) in our study tried to lose or maintain weight in the past year. The literature on weight control suggests that older people are encouraged to control weight due to health risks and medical conditions, while younger adults are motivated to control weight to improve their self-image (Faucher & Mobley, 2010). Despite the clinically required objectives of weight control, previous studies on Korean adults aged > 19 years have reported that older adults are less likely to modify their weight control behaviors than younger adults (Hwang, Ryu, & Park, 2015). Similarly, our study participants showed a decrease in weight control attempts with increasing age. The highest rate of weight control was observed in the 50s group, while the lowest rate was observed in the 70s group, even after adjusting for age, BMI, WC, and chronic diseases. The significant differences observed between age groups seem to be closely associated with socioeconomic status, such as household income and educational level, influencing health-related behaviors. Our findings imply that women in their 50s need more specific and varied ways to maintain a healthy body weight. Women in the 70s with obesity or overweight require motivation to lose body weight.
Different factors associated with weight control attempts between age groups
In the 50s group, body image was mostly associated with weight control attempts. It is rational that women with an accurate perception of body weight tend to perform more weight control measures than those who underperceive their weight (Hwang et al., 2015), as evidenced by the lower rate of weight control attempts in the older age group, where more women had an underperception of their body weight than those in the 50s group. By developing accurate weight perception, obese individuals can be motivated to engage in weight management programs (Kim, Kim, Cho, & Cho, 2008). Additionally, individuals with obesity who under-perceive their weight try less to lose weight and practice unhealthy methods for weight control, such as fasting, using laxatives, or performing induced vomiting (Jones, Grilo, Masheb, & White, 2010). Thus, accurate weight perception is necessary for developing healthy and effective weight control behaviors.
Household income was associated with weight control attempts in the 50s age group. This indicates that economic status affects weight control behaviors in middle-aged women, although they have greater household income than older women. Similarly, previous studies have reported that individuals with higher socioeconomic or educational levels are more likely to manage their weight (Wardle & Griffith, 2001). This is probably because they are knowledgeable regarding their health status and have ample access to weight management services, collectively facilitating the adaptation of good weight control behaviors (Morland, Wing, Diez Roux, & Poole, 2002). Considering that women in their 50s with obesity in the mid-high to highest quartile of household income have a greater likelihood of attempting weight control, social support for the maintenance of healthy weight in middle-aged women with low economic status should be addressed to reduce health inequality.
Lower educational level was associated with fewer weight control attempts in both the 50s and 70s groups. Particularly, women in their 70s with obesity who had an educational level higher than middle school were 5-times more likely to try appropriate weight control strategies than women with middle school or lower educational levels. Consistent with our observations, studies have reported that educational level in older adults is closely associated with preventive health behaviors, and women with low educational levels are more likely to have a higher prevalence of chronic diseases and lower quality of life than women with high educational levels (Korea Institute for Health and Social Affairs, 2017; Liu, Liu, Li, & Chen, 2015). In particular, a study comprising 3,080 women with obesity showed that low educational status is a contributing factor to the development of obesity and a higher risk for obesity-related diseases (Tanyolaç, Çikim, Azezli, & Orhan, 2008). The educational level is lower in women aged > 70 years than in other population groups (Korea Institute for Health and Social Affairs, 2017), causing this population to have low “health literacy.” (Davis, Michielutte, Askov, Williams, & Weiss, 1998) Hence, healthcare providers should offer sufficient and targeted education on healthy weight maintenance and develop better public health education materials and practical programs for older women. The lower rate of weight control attempts in the 70s group than that in the other age groups could be related to a lower education level; even after multiple logistic regression analysis adjusting for other factors, lower educational level remained a significant factor associated with weight control attempts in the 70s groups. Therefore, education for the age at which obesity leads to many metabolic and degenerative diseases is needed. Understanding the sources of information on health and health care among older women can play an important role in raising awareness regarding the risk of obesity and improving weight control behaviors. Besides healthcare providers, older adults often obtain health information from television programs, newspapers, and family or friends (Chaudhuri, Le, White, Thompson, & Demiris, 2013). Thus, it is necessary to proactively guide older adults to reliable sources of valid health information and help them avoid misinformation.
Personal weight control strategies
In this study, the methods used by most obese women trying to lose or maintain weight were associated with decreased energy intake and increased energy expenditure, consistent with evidence-based guidelines for obesity management (Seo et al., 2019). Reducing the size of meals was the most commonly practiced weight control strategy, and this practice was more prevalent in older individuals than in younger individuals. Women in their 60s and 70s more frequently chose to reduce their meal size than to perform exercise. This is probably because adjusting meal size may be easier for them than to perform exercise or because women aged > 60 years are likely to have chronic conditions, including osteoarthritis and activity limitation. However, there was no difference when comparing the mean nutritional intake of women with obesity and total women aged >50 years. Considering that women with obesity were consuming fewer calories than the estimated average requirement based on the dietary reference intakes for Koreans (1,800 kcal for women aged 50–64 years, 1,600 kcal for women aged 65+ years) (Ministry of Health and Welfare, 2015), reducing or skipping meals for weight control is not a strategy for older women with obesity and should be discouraged.
Many older women try to adjust their meal plan and rely on meal size. Therefore, physicians should discuss dietary habits with these women and determine whether they have any nutritional deficiencies before starting treatment. According to a report by the Nutritional Screening Initiative, 58.7% of adults aged 65 years or older are at risk of nutritional deficiency and need either dietary attention or improvement (Jang et al., 2019). Malnutrition in older adults can occur across the range of BMIs and is also observed in overweight or obese older adults (Winter, Flanagan, McNaughton, & Nowson, 2013). Thus, physicians should consider the potential risks of energy restriction when managing older obese individuals. Improving dietary quality by increasing the consumption of nutrient-dense and healthy foods or restricting the intake of salty and micronutrient-poor foods is considered appropriate. A healthy diet that includes high-fiber foods, such as fruits, vegetables, nuts, and whole grains, will help increase satiety and reduce excessive caloric intake in older individuals (Han et al., 2011).
Exercise was another commonly practiced method of weight control among the older women in our study. A geriatric fact sheet by the Korean National Statistics reported that older individuals spent over 8 hours sitting or lying down each day, and 51.9% exercised in insufficient amounts (Jang et al., 2019). In this report, the most common exercise method was walking (35.4%), followed by other aerobic exercises (34.4%), and only 8.4% of older women practiced resistance exercise regularly. Considering these reports and our findings, physicians need to emphasize the importance of exercise in controlling weight in older people, offer more age-appropriate physical activity and exercise options based on their chronic conditions or physical strength, and educate them to perform exercises properly.
In addition to diet and exercise, there are multiple pharmacological agents that can be used for weight loss. Interestingly, in our study, anti-obesity medications prescribed by physicians were less frequently used by women with obesity than dietary supplements, suggesting a low medication usage rate in South Korea, where several anti-obesity medications for long-term use are now available (Tak & Lee, 2021). This is possibly attributable to the fact that doctors were hesitant to prescribe anti-obesity medications to middle-aged and older people, or women with obesity were reluctant to see a doctor and get prescriptions to lose weight (Thomas, Mauer, Shukla, Rathi, & Aronne, 2016).
Limitations and strengths
This study had limitations. First, since this was a cross-sectional study, it was difficult to assign causality to determine causality between factors. Second, reporting bias cannot be ruled out, as data collection was performed through self-reported questionnaires addressing health-related factors and dietary intake. However, this study has several strengths. One of the major strengths was the large-scale, nationally representative sampling of Korean women aged ≥ 50 years. Moreover, we used the most reliable available data obtained using a variety of health-related questions and tests, which allowed us to control for various potential confounding factors associated with weight control.
Conclusions
Our study showed that the majority of middle-aged or older women with obesity try to lose or maintain weight, although these efforts decrease with increasing age. Moreover, lower educational levels and household income negatively affected weight control attempts. Reducing the size of meals and performing exercise are the most commonly practiced weight control strategies in older women with obesity. The social status of women, such as low educational level and household income was closely associated with efforts to control weight among middle-aged and older women with obesity. These findings suggest that policy support should be considered to help women with obesity continue to control weight and use healthy methods to lose weight.
Acknowledgments
This work was supported by a clinical research grant from Pusan National University Hospital in 2020 and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1G1A1008401).
References
-
Apovian, C. M., Frey, C. M., Wood, G. C., Rogers, J. Z., Still, C. D., & Jensen, G. L. (2002). Body mass index and physical function in older women. Obesity Research, 10(8), 740-747.
[https://doi.org/10.1038/oby.2002.101]

-
Chang, V. W., Asch, D. A., & Werner, R. M. (2010). Quality of care among obese patients. JAMA, 303(13), 1274-1281.
[https://doi.org/10.1001/jama.2010.339]

-
Chaudhuri, S., Le, T., White, C., Thompson, H., & Demiris, G. (2013). Examining health information-seeking behaviors of older adults. Comput Inform Nurs, 31(11), 547-553.
[https://doi.org/10.1097/01.NCN.0000432131.92020.42]

-
Davis, T. C., Michielutte, R., Askov, E. N., Williams, M. V., & Weiss, B. D. (1998). Practical assessment of adult literacy in health care. Health Education & Behavior, 25(5), 613-624.
[https://doi.org/10.1177/109019819802500508]

-
Dorner, T. E., & Rieder, A. (2012). Obesity paradox in elderly patients with cardiovascular diseases. International Journal of Cardiology, 155(1), 56-65.
[https://doi.org/10.1016/j.ijcard.2011.01.076]

-
Faucher, M. A., & Mobley, J. (2010). A community intervention on portion control aimed at weight loss in low-income Mexican American women. Journal of Midwifery & Women‘s Health, 55(1), 60-64.
[https://doi.org/10.1016/j.jmwh.2009.03.014]

-
Han, T. S., Tajar, A., & Lean, M. E. (2011). Obesity and weight management in the elderly. British Medical Bulletin, 97(1), 169-196.
[https://doi.org/10.1093/bmb/ldr002]

-
Hwang, J. H., Ryu, D. H., & Park, S. W. (2015). Interaction Effect between Weight Perception and Comorbidities on Weight Control Behavior in Overweight and Obese Adults: Is There a Sex Difference? Journal of Korean Medical Science, 30(8), 1017-1024.
[https://doi.org/10.3346/jkms.2015.30.8.1017]

-
Jang, I. Y., Lee, H. Y., Lee, E., & 50th Anniversary Committee of Korean Geriatrics Society. (2019). Geriatrics Fact Sheet in Korea 2018 From National Statistics. Annals of Geriatric Medicine and Research, 23(2), 50-53.
[https://doi.org/10.4235/agmr.19.0013]

-
Jones, M., Grilo, C. M., Masheb, R. M., & White, M. A. (2010). Psychological and behavioral correlates of excess weight: misperception of obese status among persons with Class II obesity. International Journal of Eating Disorders, 43(7), 628-632.
[https://doi.org/10.1002/eat.20746]

-
Kim, D. S., Kim, H. S., Cho, Y., & Cho, S. I. (2008). The effects of actual and perceived body weight on unhealthy weight control behaviors and depressed mood among adult women in Seoul, Korea. Journal of Preventive Medicine and Public Health, 41(5), 323-330.
[https://doi.org/10.3961/jpmph.2008.41.5.323]

- Korea Institute for Health and Social Affairs. (2017). National Survey of Older Koreans-Findings and Implications. Retrieved April 17, 2020, from https://www.kihasa.re.kr/web/publication/newbooks_pdsissue/view.do?menuId=46&tid=71&bid=200&ano=1487
-
Kweon, S., Kim, Y., Jang, M. J., Kim, Y., Kim, K., Choi, S., . . . & Oh, K. (2014). Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). International Journal of Epidemiology, 43(1), 69-77.
[https://doi.org/10.1093/ije/dyt228]

-
Lavie, C. J., De Schutter, A., Patel, D., Artham, S. M., & Milani, R. V. (2011). Body composition and coronary heart disease mortality--an obesity or a lean paradox? In Mayo Clinic Proceedings, 86(9), 857-864.
[https://doi.org/10.4065/mcp.2011.0092]

-
Liu, Y. B., Liu, L., Li, Y. F., & Chen, Y. L. (2015). Relationship between Health Literacy, Health-Related Behaviors and Health Status: A Survey of Elderly Chinese. International Journal of Environmental Research Public Health, 12(8), 9714-9725.
[https://doi.org/10.3390/ijerph120809714]

-
Lopez-Garcia, E., Banegas Banegas, J. R., Gutierrez-Fisac, J. L., Perez-Regadera, A. G., Ganan, L. D., & Rodriguez-Artalejo, F. (2003). Relation between body weight and health-related quality of life among the elderly in Spain. International Journal of Obesity Related Metabolic Disorders, 27(6), 701-709.
[https://doi.org/10.1038/sj.ijo.0802275]

- Ministry of Health and Welfare. (2015). The Korean Nutrition Society, Dietary Reference Intakes for Koreans. Retrieved April 22, 2019, from http://www.kns.or.kr/FileRoom/FileRoom_view.asp?idx=79&BoardID=Kdr, .
-
Moredich, C. A., & Kessler, T. A. (2014). Physical activity and nutritional weight loss interventions in obese, low-income women: an integrative review. Journal of Midwifery & Women‘s Health, 59(4), 380-387.
[https://doi.org/10.1111/jmwh.12061]

-
Morland, K., Wing, S., Diez Roux, A., & Poole, C. (2002). Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine, 22(1), 23-29.
[https://doi.org/10.1016/S0749-3797(01)00403-2]

-
Piercy, K. L., Troiano, R. P., Ballard, R. M., Carlson, S. A., Fulton, J. E., Galuska, D. A., George, S. M., & Olson, R. D. (2018). The Physical Activity Guidelines for Americans. JAMA, 320(19), 2020-2028.
[https://doi.org/10.1001/jama.2018.14854]

-
Romero-Corral, A., Montori, V. M., Somers, V. K., Korinek, J., Thomas, R. J., Allison, T. G., . . . Lopez-Jimenez, F. (2006). Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet, 368(9536), 666-678.
[https://doi.org/10.1016/S0140-6736(06)69251-9]

- Rural Development Administration, National Institute of Agricultural Sciences. (2018). Korean Standard Food Composition Table the 9th Revision. Rural Development Administration, National Institute of Agricultural Sciences: Wanju, Korea. Retrieved March 2, 2020, from http://koreanfood.rda.go.kr/eng/fctFoodSrchEng/engMain
-
Santos, I., Sniehotta, F. F., Marques, M. M., Carraca, E. V., & Teixeira, P. J. (2017). Prevalence of personal weight control attempts in adults: a systematic review and meta-analysis. Obesity Reviews, 18(1), 32-50.
[https://doi.org/10.1111/obr.12466]

-
Seo, M. H., Lee, W. Y., Kim, S. S., Kang, J. H., Kang, J. H., Kim, K. K., & Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity (2019). 2018 2018 Korean Society for the Study of Obesity Guideline for the Management of Obesity in Korea. Journal of Obesity & Metabolic Syndrome, 28(1), 40-45.
[https://doi.org/10.7570/jomes.2019.28.1.40]

-
Shim, J. S., Oh, K., & Kim, H. C. (2014). Dietary assessment methods in epidemiologic studies. Epidemiology and Health, 36, e2014009.
[https://doi.org/10.4178/epih/e2014009]

-
Tak, Y. J., & Lee, S. Y. (2021). Anti-Obesity Drugs: Long-Term Efficacy and Safety: An Updated Review. The World Journal of Men‘s Health, 39(2), 208-221.
[https://doi.org/10.5534/wjmh.200010]

- Tanyolaç, S., Çikim, A. S., Azezli, A. D., & Orhan, Y. (2008). Correlation between educational status and cardiovascular risk factors in an overweight and obese Turkish female population. Anatolian Journal of Cardiology/Anadolu Kardiyoloji Dergisi, 8(5), 336-341.
-
Thomas, C. E., Mauer, E. A., Shukla, A. P., Rathi, S., & Aronne, L. J. (2016). Low adoption of weight loss medications: A comparison of prescribing patterns of antiobesity pharmacotherapies and SGLT2s. Obesity (Silver Spring), 24(9), 1955-1961.
[https://doi.org/10.1002/oby.21533]

-
Wardle, J., & Griffith, J. (2001). Socioeconomic status and weight control practices in British adults. Journal of Epidemiology & Community Health, 55(3), 185-190.
[https://doi.org/10.1136/jech.55.3.185]

-
Weinheimer, E. M., Sands, L. P., & Campbell, W. W. (2010). A systematic review of the separate and combined effects of energy restriction and exercise on fat-free mass in middle-aged and older adults: implications for sarcopenic obesity. Nutrition Reviews, 68(7), 375-388.
[https://doi.org/10.1111/j.1753-4887.2010.00298.x]

-
Westerterp, K. R. (2018). Changes in physical activity over the lifespan: impact on body composition and sarcopenic obesity. Obesity Reviews, 19 Suppl 1, 8-13.
[https://doi.org/10.1111/obr.12781]

-
Winter, J., Flanagan, D., McNaughton, S. A., & Nowson, C. (2013). Nutrition screening of older people in a community general practice, using the MNA-SF. The Journal of Nutrition, Health & Aging, 17(4), 322-325.
[https://doi.org/10.1007/s12603-013-0020-0]

- World Health Organization. (2020). Obesity and overweight. Fact sheet. Retrieved April 2, 2020, from https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
-
Yaemsiri, S., Slining, M. M., & Agarwal, S. K. (2011). Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003-2008 Study. International Journal of Obesity(Lond), 35(8), 1063-1070.
[https://doi.org/10.1038/ijo.2010.229]

Biographical Note: Jong-Hwan Park is an assistant professor at Health Convergence Medicine Laboratory, Biomedical Research Institute, Pusan National University Hospital, Korea. His academic interest is in smart health care, clinical behavioral medicine, physical activity and health. Email: parkj@pusan.ac.kr
Biographical Note: Young Jin Tak is an associate professor in the Department of Family Medicine, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, South Korea. Her academic interest is in metabolic diseases, obesity, nutrition, and smart health care. Email: 03141998@hanmail.net
Biographical Note: Seung Hwan Song is a professor in the Department of Thoracic and Cardiovascular Surgery, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, South Korea. His academic interest is in cardiac surgery for heart failure, e.g. heart transplantation and mechanical circulatory support. Email: song77.sh@gmail.com
Biographical Note: Up Huh is an assistant professor in the Department of Thoracic and Cardiovascular Surgery, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, South Korea. His academic interest is in vascular surgery & intervention, central venous catheter for chemotherapy, aging, well-being, and screening of vascular disease. Email: tymfoo82@pusan.ac.kr
Biographical Note: Baek Vin, Lim is a professor in the Department of Physical Education, College of Bio-health at DongSeo University, South Korea. His academic interest is in physical education, sports medicine, exercise prescription, public health and welfare, digital healthcare. Email: todd64@ naver.com