Myths and Misconceptions about Sexual and Reproductive Health among Indigenous Women—An Intergenerational Study using Dyadic Interviews
Abstract
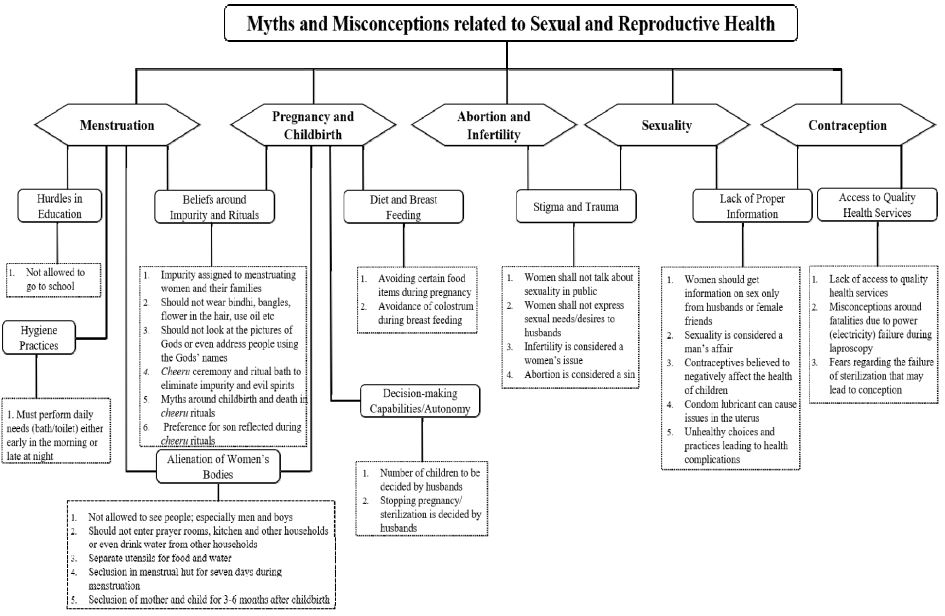
This study explores the prevalence of myths and misconceptions and their impact on indigenous women’s sexual and reproductive health. It was conducted in Attappady, a tribal block in the Palakkad district of Kerala, a state in southern India, which has been in the news in relation to maternal and child health issues. Forty-five dyadic, in-depth, face-to-face interviews with indigenous women from two generations were used for data collection, followed by thematic analysis. Intergenerational changes in the lived experiences of indigenous women are minimal, and comparative analysis shows the existence of gender-power relations. The analysis revealed inadequate information on sexual and reproductive health rights, inaccessibility and unavailability of sexual and reproductive health services, unequal relationships with partners, fear of social exclusion, and high sensitivity toward traditional practices embedded in sociocultural systems. The interplay between gender and cultural and health inequalities determines the propagation and sustaining of myths and misconceptions, resulting in the denial of sexual and reproductive health rights.
Keywords:
Sexual and Reproductive Health Rights, indigenous women, intergenerational, dyadic interviews, myths and misconceptionsIntroduction
More than 25 years have passed since the International Convention on Population and Development (ICPD), a comprehensive global effort, laid the foundations of Sexual and Reproductive Health Rights (SRHR). The ICPD conceived and defined SRHR as a human right and emphasized the necessity of ensuring universal access to SRHR. Moreover, when the Sustainable Development Goals (SDGs) were codified in 2015 (United Nations, 2015), three of the 17 goals were linked to the advancement of SRHR. These were: ensure healthy lives and promote well-being for all at all ages (SDG 3); ensure inclusive and equitable quality education and promote lifelong learning opportunities for all (SDG 4); and achieve gender equality and empower all women and girls (SDG 5) (Galati, 2015).
SRHR includes an array of rights for women: these include the right to seek, receive and impart information related to sexuality education; choice of partners; consensual sex and marriage; to have safe, effective, affordable and acceptable family planning methods of their choice; and the right to safe pregnancy and birth. Since the SRHR ensures access to and control over a set of daily life choices and experiences concerning menstruation, sexuality, partner choice, family planning, and maternal and child health, investing in women’s health, education, and empowerment is critical for ensuring them. Poor SRHR services leads to unintended pregnancies, complications in maternal and child health, unsafe abortions, gender-based violence, sexually transmitted diseases, and reproductive health issues (Starrs et al., 2018). Most of these complications have intergenerational effects; thus, complete access to sexual and reproductive health rights is a critical element in achieving SDGs. However, the denial of sexual and reproductive health rights remains prevalent worldwide (UN Office of the High Commissioner for Human Rights, n.d.).
The indigenous 1) communities represent 8.6% of India’s population (Office of the Registrar General & Census Commissioner, India, 2011) and intra- and inter-state variations exist between different indigenous populations in terms of socioeconomic and cultural diversity. A 2016 Lancet study revealed that the Infant Mortality Rate (IMR) among the tribal population in India is the second highest among tribal populations worldwide (Anderson et al., 2016). As per the report of the Expert Committee on Tribal Health in 2018, the IMR and Under-five Mortality Rate (U5MR) for tribal populations have reduced significantly over a quarter century. The IMR in India’s tribal population has nearly halved; however, the gap with other social groups has widened from 10% to 38%. The U5MR also showed a 58% decline; again, however, the gap with other social groups widened from 21% to 48% (Ministry of Health and Family Welfare, 2018). According to the National Family Health Survey–5, the IMR among the tribal population stands at 42 deaths per 1000 live births and the U5MR at 50 deaths per 1000 live births. It also shows that 72% of tribal children, 65% of tribal women, and 33% of tribal men are anemic, which is the highest among all social groups (International Institute of Population Sciences, 2021).
Attappady, a tribal block in Kerala, India, has been criticized worldwide for its increasing rates of infant mortality and malnutrition (Manikandan, 2014). The Logical Indian (Nazir, 2022) reported that the State Integrated Tribal Development Programme has estimated at least 137 infant deaths, 300 abortions, 90 intrauterine deaths, and 21 stillbirths in Attappady since 2012. The majority of tribal mothers are anemic and lack the nutrition required to give birth to a healthy child; thus, the average infant weighs around 600–800 g at birth and most of the children are affected by intrauterine growth retardation (Pariyaram Medical College, 2016). Murshid and Krishnaprabha (2018) also highlighted how malnutrition among tribal women results in miscarriages and low birth weight.
The sexual and reproductive health experiences of women and girls vary across communities, and indigenous women are more vulnerable than any other population. Ignorance and superstition rooted in unwritten cultural beliefs and traditional practices are the major factors that contribute to their backwardness and vulnerability (Deogaonkar, 1990). Fear of the social exclusion that may result from the violation of cultural practices forces them to sustain their rituals. Although menstruation is associated with maturity and fertility, notions of impurity, curses, and sin are invoked to control the female body and mind. Sociocultural taboos and myths associated with menstruation sometimes result in unhygienic personal care among women and girls, who follow those practices unquestioningly (Dhingra, Kumar, & Kour, 2009). From an intergenerational perspective, younger girls find these myths and taboos outdated and objectionable compared to older adults (Asmat, Manhas, Sharma, Fatima, & Hassan, 2020).
Similarly, socio behavioral factors and cultural beliefs among tribal people lead to lower rates of contraceptive use. In addition, women lack proper information about and access to modern contraceptives, making them more vulnerable in their family planning choices and decisions. These circumstances underline the need for a culturally sensitive approach to indigenous women and ensuring their access to locally appropriate contraceptive methods to improve their sexual and reproductive health outcomes (Palo, Samal, Behera, & Pati, 2020).
Pregnant women in these communities believe in age-old practices and use traditional rituals during pregnancy and childbirth (Sengupta, 2019). They believe that such rituals are important for maternal and child well-being. Cultural practices and beliefs are strong among such communities, and research has revealed their negative impact on pregnancy and childbirth outcomes, such as maternal and child care, institutional delivery, breastfeeding, and antenatal care (Hansdah & Rath, 2021; Thipanyane, Nomatshila, Oladimeji, & Musarurwa, 2022). These practices and beliefs include ritual pollution during pregnancy and childbirth, isolation of the mother and newborn, avoidance of certain foods during pregnancy and lactation, discarding colostrum, and not breastfeeding the infant for a period of time after birth (Bandyopadhyay, 2009).
The traditional practices, cultural contexts, and individual perceptions are the key features that shape the sexual and reproductive health experiences of indigenous women in Odisha (Palo et al.,2020). In another study in Kargil district, India, the authors opined that older generations, particularly grandmothers and mothers, believe and follow these myths and misconceptions even though they are not sure about their viability (Asmat et al., 2020). A recent study conducted in Wayanad district, a major tribal belt in Kerala, found that several rituals followed by tribal communities have a gendered dimension that is mostly centered on the woman’s body, especially reproductive aspects such as menstruation, marriage, pregnancy, and childbirth. Although indigenous cultures and traditions need to be preserved, unnecessary harmful practices, myths, and misconceptions that hinder indigenous women’s access to sexual and reproductive health should be addressed (Rajitha & Kuruvilla, 2021).
An analysis of the myths and misconceptions regarding the sexual and reproductive health of indigenous women in Attappady would help us understand the maternal and child health complications that persist in the area. In addition, a comparative analysis of intergenerational changes would provide a better understanding of lived experiences regarding the same. In this respect, the present intergenerational study is contextualized among indigenous women in Attappady, focusing on myths and misconceptions related to sexual and reproductive health experiences. This is the first study to conduct in-depth, face-to-face dyadic interviews with mothers and grandmothers from an intersectional perspective, thereby enriching feminist scholarship related to doubly marginalized indigenous women.
Methods
Feminist qualitative research originates from the understanding that all knowledge is positioned in the bodies and subjectivities of people, especially in the cases of women and marginalized groups; truth and knowledge are inseparable from the lived experiences of the researched (Haraway, 1988). This study explores the nature of myths and misconceptions related to sexual and reproductive health experiences among tribal women in Attappady. Exploring and understanding these experiences by comparing intergenerational changes from a feminist intersectional perspective provides further insight into how to address the existing gaps in the system.
A researcher enters the field and accesses the participants with the help of gatekeepers, who are usually people in managerial positions or field-level workers who have access to both the field and potential participants (Bell, 2014). As the study participants belonged to vulnerable indigenous communities, such as Irula, Muduga, and Kurumba, permission had to be obtained from government institutions at various levels. Ensuring the participation of all indigenous communities in the block was challenging as some lived in remote forest areas, which required further permission. The permission guidelines specified that the researcher could access the field only through field-level workers.
Ethical approval was obtained from the Calicut University Ethics Committee for Human Research. The researcher explained the nature and purpose of the study to the participants through a detailed participatory information sheet. Informed consent was obtained from all participants, and the interviews were audio-recorded with their permission. The anonymity of all participants was guaranteed by using pseudonyms ensuring that the reported quotes and incidents were not traceable to individual participants.
The eruption of the COVID-19 pandemic during the field work made the procedure more complicated and time-consuming. Pandemic protocols were strictly followed during data collection. Necessary protective measures were taken by the researcher during fieldwork, such as the use of face masks and hand sanitizers, isolating herself if symptoms were observed, and conducting occasional RT-PCR tests.
This descriptive study was conducted from December 2021 to May 2022. The researcher acknowledges the help of the gatekeepers in this study whose involvement and guidance helped the researcher enhance her field knowledge. It should, however, be noted that although multiple-level monitoring was intended to ensure the safety of the researcher and the subjects, the involvement of gatekeepers in deciding the participants might have affected access to potential subjects and the research outcomes. The gender dynamics of gatekeeping also came into play as a few younger women found it difficult to share their experiences in the presence of male gatekeepers. However, the researcher would like to express her appreciation for their field experience and work integrity.
Interview locations and times were mutually agreed with the participants. As the research dealt with emotional and sensitive personal experiences, the participants may not have felt comfortable talking in public; therefore, priority was given to their convenience. Most interviews were conducted at their residences, and others at the workplace, community centers, and similar locations as respondents preferred. The researcher gradually gained the trust of the tribal women and was able to build a rapport with them. The researcher also made conscious efforts in dress and appearance; churidars and kurtas were worn as they exuded familiarity and had a positive effect during fieldwork.
Forty-five dyads (each consisting of a younger mother along with her mother or mother-in-law) were purposively selected for in-depth, face-to-face interviews. An interview guide was constructed based on the available literature, and the interviews were conducted in the regional language. The researcher allowed respondents to speak naturally and with limited intervention. The researcher also conducted ten case studies to substantiate the data collected through in-depth interviews. Conducted in regional languages, the interviews were transcribed and translated into English. The data were subjected to thematic analysis using inductive coding, a ground-up approach in which codes and themes are derived from raw data, in this case the in-depth interviews and case studies of indigenous women.
“Intersectionality has become a predominant way of conceptualizing the relation between systems of oppression which construct our multiple identities and our social locations in hierarchies of power and privilege” (Carastathis, 2014, p. 304). Power is central to intersectional analysis and plays a critical role in creating and perpetuating personal and social structures of discrimination and oppression (Women's Health Research Network, 2009). An intracategorical approach focuses on one social category at the intersection of multiple social identities (McCall, 2005). Thus, intergenerational changes in myths and misconceptions regarding the sexual and reproductive health experiences of indigenous women in Attappady were analyzed from an intersectional perspective.
Results
Myths and Misconceptions Related to Menstruation
Even though menstruation is a biological process, the cultural importance of the cheeru ceremony, which celebrates a girl’s first menstruation, is deeply embedded in the cultural and social system. Usually, cheeru is performed on the seventh day of menstruation, but it has to be conducted within one year of a girl’s menarche. It is believed that cheeru alone redeems them from the impurities introduced by menstruation. For the first seven days of her period, a girl must stay confined in the kudusu , a small hut made of palm leaves, fig leaves, and bamboo sticks, palm leaves being a symbol of purification. Usually, it is built outside the home, but nowadays, as people live in hamlets and the houses are situated close to one another, which limits courtyard space, families have to create a space for the kudusu inside the house.
In most cases, the girl remains alone in the menstrual hut, but sometimes her maternal cousins or sisters-in-law accompany her. She is not allowed to go to school for the seven days, is given food and water in separate utensils, should not wear a bindhi (an ornamental dot on her forehead), bangles, or flowers, and should not oil her hair. She is only allowed to bathe either early in the morning or late at night without being seen by anyone, especially boys and men. She must travel to the nearest stream or river but if this is far away, she is allowed to bathe in the courtyard.
If the family lacks the money to conduct the cheeru, they can perform a ritual to let her enter the home, but the function must be conducted within a year for purification. Otherwise, the family members are ostracized and forbidden from entering other houses or temples or dining with others. According to their belief, the gods can take the form of any random thing like a snake or mud pot, which prevents them from venturing outside or to any other house. Every house has a daivaveedu (prayer room) that must be kept pure. Hence, people from a menstruating girl’s house do not enter other people’s houses. If they do so, they believe that they will be cursed and something bad will occur.
It is mandatory to eliminate the theetu (impurity). On the seventh day, the girl is taken to the nearest stream or river by female relatives or friends for a ritual bath. She is then allowed to use oil, turmeric, etc. for bathing. After the bath, a green leaf called tadisi or chadichi is used to drive out any evil spirit from the girl’s body. The chadichi leaves are collected from the river bank, the veins separated from the leaves, and the veins woven around the girl’s body, from head to toe. The girl digs a shallow pit in the soil where she stands and in which she buries the leaf veins. This removes impurities and drives out evil spirits. If the leaf veins are not buried properly and comes out, the evil spirit is considered to be still with her and she must do it again.
After the ritual bath, they burn all the dresses and kudusu and throw the ashes in the river. They smear the house courtyard with a paste of cow dung and hang chadichi leaves to purify the place. As part of the rituals at home, the girl carries several items, such as fruits, grains, leaves, flowers, and beauty products, in her saree pallu (the loose end of a saree) or in a shallow basket made of bamboo. She also carries a child in one hand and pounds on a mortar with a pestle. The child is chosen from among her immediate family members; there is a preference for male children aged between two and three and if a boy cannot be found, a girl is carried. If the girl carries a boy, they believe she will give birth to a baby boy, and to a baby girl if she carries a girl. The ritual must be carried out carefully without dropping any of the things from the saree pallu; if the girl drops anything, it is supposed to bring bad luck, and will lead to the death of her first child. According to Kavya, “if anything spills, she will lose her first child. It could be an abortion, miscarriage, stillbirth, or even child death. It has happened in our hamlet.” She was serious and certain in her statements and also offered proofs for her arguments. After the ritual, the girl enters the house and a feast is given to the people of the hamlet, called oru nazhi arivaykkal, as a token of sharing the family’s happiness. It is the responsibility of the maternal uncles and aunts to conduct this function: they buy clothes, ornaments, and sweets for the girl, and she is dressed up like a bride.
Even after the first menstruation, women have to practice separation for the first seven days of each period. They are not supposed to go to the kitchen or daivaveedu during this time, nor can they cook or be with their husbands. They must not see other men and must not address anyone using the names of the gods. Nowadays, because there are more nuclear families, men cook during the wife’s period, and women do other household chores, such as cleaning and washing clothes.
Myths and Misconceptions about Sexuality
It was not easy for respondents to talk about sexuality. They see it as shameful for women to talk publicly about these issues. Most of the women responded “It is the men’s matter and we do not like to talk about those things.” They believe that sexuality is a private affair, and that women should learn and clarify doubts about sexuality from their husbands. Malika, a 26-year-old Muduga woman, said, “If they had any doubts about sex, the husband would ask his close friends or seek information on Google or YouTube. Network coverage is low in our hamlet, so my husband goes to the nearby hill to get better connectivity and later shares the information with me.”
Only a few people reported discussing SRHR-related doubts with their friends during leisure time without being noticed by older adults. Nachi, an elder woman aged 48, shared that, “In those times, we had no mobile phone, we were afraid of discussing anything with our husbands and we believed that we should not ask them, we had to understand it on our own. So, I used to talk with my close friend, who was married, and came to understand all these things.”
Some women said that expressing sexual needs to their husbands was sometimes problematic. According to Bina, a 26-year-old Muduga tribal woman, “We usually do not ask for it; we let them decide. If they express their wishes, we are happy to go along. But if we express our wishes, they might not listen to us. They would start wondering whether we are having an affair with someone if we do not consent when they wish to have it.”
Myths and Misconceptions about Contraception
Myths and misconceptions related to contraception are prevalent among indigenous women. Many are concerned that contraceptives, especially artificial contraceptives, can cause health problems for women and children. Many of them shared their negative experiences with the Copper T intrauterine device and reported health issues such as weight loss, heavy and irregular bleeding, back pain, vomiting, urinary infection, and inability to lift heavy objects. Misconceptions created by stories of Copper T going missing inside the uterus and other dangers of contraceptives, including their degrading effect on the health of future children, are still prevalent. In contrast to younger women’s misapprehensions, a few elderly women shared that they would have used contraceptives to avoid unwanted pregnancies if they had known about those methods in the past.
Mani, a 49-year-old Muduga woman with four children, narrated her experiences. She had her first child within one year of marriage. She said, “I was eating good food and conceived quickly after marriage. Therefore, the health workers advised us to practice child spacing. My husband is a good man. He knew about Nirodh [a type of condom] from the newspaper, bought it from a medical store, and we decided to use it for birth spacing. It was for our children’s health and mine.” During the fourth pregnancy, a cyst was found in her uterus. She said, “I thought, maybe my uterus’ condition was triggered by the use of Nirodh. There is an oil in it, right? No one told me this could be the reason for the cysts, but I believe so.” She finally went to a medical college and had a hysterectomy.
Some tribal women believe that children are God’s blessing, so there is no need for contraception, particularly artificial methods. According to them, natural methods of contraception are appropriate for achieving spacing between children, and they are safer methods as there is no harm to the body. They added that men are mostly reluctant to use condoms, denying them complete contraceptive protection. Sudha, a 36-year-old Muduga woman, worked as Scheduled Tribal (ST) promoter for four years. She was part of the Kudumbasree (the largest women’s network in the world, started as an anti-poverty program in Kerala) and MGNREGA programs (the Government of India’s social security program that ensures “right to work” by providing at least 100 days of wage employment per year). She has five children, of which only four are alive. She had heard of contraceptives, but did not know about any of these methods. She said, “It will cause health problems to children, right? So, we decided not to use it. For child spacing, we used abstinence.” Vaginal penetration was deliberately avoided when abstinence was not possible. Although she worked as an ST promoter for years and was an influencer, she had several misconceptions regarding contraception. She had heard about negative impacts on health caused by the use of contraceptives such as Copper T, such as weight loss, back pain, and infections, and feared that the artificial methods inserted in the body could negatively affect children’s health. She actively participated in social networking platforms, which have the potential for behavioral change and transformation. When both the misconceptions and the positive social exposure were taken into consideration, the misconceptions triumphed and the outcome was a forgoing of sexual and reproductive health rights.
In contrast, Rani, a 23-year-old Muduga woman with an unplanned second pregnancy, wanted to stop further pregnancies through sterilization. However, she was denied the procedure as the hospital staff told her that she was still young, and she has to wait until she reaches the age of 27. She was prescribed contraceptives to avoid an unwanted pregnancy. Earlier, she had used Copper T; however, due to infections, it had been removed. Although she had heard of condoms, her husband was not comfortable with them. Later, she received a contraceptive injection, which was administered once every three months at the government hospital, 30 km away from her home. It was difficult for her to reach the hospital every three months for the dosage, but her determination was exemplary. In this case, the tribal woman somehow overcame the prevalent myths and misconceptions surrounding contraception. However, the lack of access to quality contraceptive services has become a major challenge.
Many indigenous women expressed concerns about female sterilization procedures. Within the community, they have heard about two types of sterilization procedure: the first one is the “current operation,” a term the women use to refer to laparoscopy and the other is the “kai operation,” the term for a mini-laparotomy (performed through a small cut in the abdomen). They have heard stories about women dying during the “current operation” (laparoscopy) and are scared to go for that, so they prefer the “kai operation” (mini-laparotomy). They fear that a power failure during the laparoscopy procedure would be harmful or even fatal. They also doubted the success of the procedure, thinking it might fail and lead to an undesired pregnancy in the future. Many misconceptions are so widespread that women prefer doctors to perform mini-laparotomies even after a normal delivery.
Bhagya, a 49-year-old Irula woman who had undergone laparoscopy, described her experiences with a smile, excitement, and relief. She went alone to have the surgery performed. “I was watching it keenly, and we (another woman from a neighboring hamlet) were praying to God for a continuous power supply. We were afraid that if the electricity went, we would die. There was a woman on the bed next to me, covered in white cloth. I think she might have died because of a power failure.” She described her experience in the operating theatre for a long time.
Chinnamma, a 39-year-old Irula woman who was working as an MGNREGA “mate” (supervisor), had four deliveries: one was a still birth and the other three children were born healthy. All of them were normal deliveries and she had not used any contraceptives for birth control or child spacing. She underwent sterilization and opted for a mini-laparotomy. She says, “I stopped pregnancy by undergoing the ‘kai operation’ as I was scared of the ‘current operation.’ We had enquired of people about the procedure and they told me that there were several risks involved in the ‘current operation.’ What if there is an electricity failure? What if we get pregnant again? It was like a C-section, I had to take a minimum of three months’ rest, and still, I have pain in those parts while doing heavy work, but it is better than dying, and I also do not want to get pregnant again.”
Myths and Misconceptions about Pregnancy and Childbirth
A majority of the women said that they have three months of “pela,” a post-delivery ritual where they have to stay separate for a period of three to six months. Earlier, the mother and child used to stay separately in a hut for six months, but now, due to shortage of space, it is in a part of the house, usually a room or hallway, depending on availability.
According to Thulasi, “We sit in the hall and the family members give us food and clothes. We use separate utensils; visitors are allowed to stand at the door and watch the mother and child. We should not enter the kitchen or the prayer room, nor should we touch anybody else. In some cases, the father stays with them for their immediate needs; he sleeps on the floor and the mother and child sleep on the cot.”
This ritualistic separation is believed to be beneficial for the mother and child as it offers protection from unwanted infections. Pregnant women avoid certain food items like gram, meat, and certain vegetables believing that “it will be harmful for the children resulting in swelling or burns on their bodies.” Bhagya, a 49-year-old Irula woman, talked about the time when they used to avoid colostrum, the first form of breastmilk produced by the mother. However, nowadays, people receive awareness classes about this from health workers, leading to favorable outcomes. This represents a positive behavioral change among young mothers in relation to the myths and misconceptions of post-delivery care.
Women lack the decision-making power to determine the number of children. They are under the misconception that the decision-making capacity always lies with the husband. Mala, a 33-year-old Irula woman with two children had wanted to avoid any future pregnancies but was unsure. She said, “My husband says not to stop getting pregnant, though I want to. I only wanted two children, but what could I do? We have to obey our husbands. So, I cannot say no to him.” Thumba, a 33-year-old Irula woman with three children, also shared her experiences. In her first marriage, she had one boy child and he is currently living with her first husband. After their separation, she married again and had two daughters from the union. When asked about family planning, she had no idea about it, and her hus-band’s decision would be the final word. “I do not know. Whatever he demands, I will follow that.”
Many women revealed their helplessness, saying that they were trying for one more child just because their husbands wished to. Madhu, a 30-year-old Muduga woman, had two children; she had lost two others, one a miscarriage and the other a premature death. She did not want another child, but her husband wanted more children. “I do not have the courage to talk to him, he will scold me, so I am keeping quiet.” When asked about contraceptives, she said that she was uncomfortable with them and had not used them at all. She had four deliveries, and only two of the children were alive. She was concerned about her health and that of her children and did not wish to go through the trauma again. She wanted to have surgery to avoid future pregnancies. In this case, the woman was sure of what she wanted, but as she believed that the final decision would be her husband’s, she was in a dilemma and faced many uncertainties about her reproductive life.
Myths and Misconceptions Related to Infertility
Suja, a 31-year-old Irula woman, had studied till class 10 and her husband, aged 38, was a coolie (unskilled laborer) with no formal schooling. They had two children, a boy of four and a girl of one and half. They had their first child after eight years of marriage. When she married, she was working for a daily wage. “I used to go for construction work; I had to carry a heavy load on my head, and it was a hard job. I think because of that I could not conceive easily,” she said. Therefore, they took advice from a doctor and she was asked to avoid lifting heavy loads. She left the job when she was the sole breadwinner of the family because her husband was not working then. She later became pregnant. Similarly, Mala, a 33-year-old Irula woman, whose husband was a 37-year-old coolie, had not conceived for six years after marriage. “I used to feel sad when people asked about children. But I did not do any poojas [a form of ritual worship] for that, I just prayed to God.” They had a 5-year-old son and she was six months pregnant at the time of the interview.
In both these cases, the women were also victims of stigma and violence from their mothers-in-law as well as society. The pressure to conceive is immense, and if women fail to do so, it often creates chaos in their lives. Conception is seen as a woman’s sole responsibility, and infertility in women causes society to view them as a liability. Such women reported trauma following the efforts of the family to disown them and to get their husbands to remarry.
Myths and Misconceptions Related to Abortion
Many women believe that the children in Attappady are gifts from Malleswaran or Lord Shiva and they have no right to decline his prasadam (blessing) through abortion. However, a few women had undergone abortions due to unfavorable situations such as their husbands’ alcoholism and violent behavior and poverty.
A 28-year-old Irula tribal woman who was a B.Ed. drop out, married a man who had quit his B. Tech course. Their marriage was planned at first, but later the families decided not to proceed with it. However, the couple continued their relationship, and the girl became pregnant. The families allowed them to marry, and as the pregnancy progressed, scans and checkups at the government hospital revealed that the fetus had acute heart issues. They were advised to abort the pregnancy, but the couple decided to proceed. “We did not want to abort the child. It is a sin. After all, he was our first child. He was God given, right? Therefore, we decided to keep him. We continued to stay at the hospital after the delivery. The baby died after 10 days. It was traumatic for us. We tried for another child only after two years.” This decision was their personal choice, which was based on their myths and misconceptions about the process of pregnancy and abortion. In India, medical termination of pregnancy is legally permitted when the fetus has chronic diseases. However, the couple decided to go through a difficult time. They said that they still carried the trauma of the loss but were relieved that their consciences were clear. Moreover, they believe birth and death are all decided by God.
Discussion
The beliefs regarding the impurity attributed to sexual and reproductive health events, such as menstruation, pregnancy, and childbirth, are still prevalent among indigenous communities. They fear being divinely cursed if they violate the rituals; for instance, the taboos on seeing men, entering the kitchen or prayer room, looking at pictures of deities, or calling people with the names of the gods during menstruation. Even when developmental efforts focused on education, infrastructure, livelihood, and health claim to have made progress in communities (Nair & Saisree, 2021), superstitious beliefs about evil spirits continue to exist. All the rituals surrounding women and reproductive events bring about the alienation of women’s bodies. Most women see the rituals as cultural and spiritual events and are unaware of the human rights violations and exclusions occurring around them. Moreover, an unhealthy diet and unhygienic practices during menstruation, pregnancy, and childbirth adversely affect the physical and mental health of both women and their children. Similar findings have been reported previously (Bandyopadhyay, 2009; Begum, Sebastain, Kulkarni, Singh, & Donta, 2017; Hansdah & Rath, 2021).
The only concern expressed by young mothers was the declining age of first menstruation and the girls’ inability to understand the importance of cultural practices related to it. Otherwise, communities strongly advocated the preservation of such rituals. Local and cultural beliefs around SRHR determine the behaviors and choices of indigenous women (Srivastava & Sahu, 2022). However, a method of addressing or abandoning harmful practices in a culture without losing the aspects of meaning and harmony is required (Kaur, 2019).
Along with these myths, there is a widespread misconception among indigenous women that girls and women must remain ignorant about sexuality. Only a few women opened up about sexuality-related experiences. Most were shy and needed time to articulate their thoughts. They also thought that talking about or expressing their sexual needs to their husbands would lead to misunderstandings in their marital relationship. These misconceptions about sexuality deny the fulfilment of women’s sexual needs and undermine their right to sexual knowledge.
Palo et al. (2020) reported that indigenous women are reluctant to adopt permanent family planning methods because of the fear of a cultural ban on worship and also worry that such methods would lead to sexual dissatisfaction. In contrast, several respondents in the present study were willing to adopt permanent family planning methods. However, the prevailing misconception that contraceptives cause health issues for women and their children holds some women back from using contraceptives. Similar findings were reported in another study (Adongo et al., 2014) where the respondents shared their health concerns over the use of contraceptives. This study underlines the role of cultural beliefs in formulating perceptions and determining the use of family planning methods. Irrational choices, decisions, and practices, such as preference for the “kai operation” over the “current operation” in sterilization due to fear, at times lead to physical and mental health complications.
The role of indigenous women in reproductive decisions related to the number of children, spacing, and sterilization is also influenced by the myths and misconceptions prevalent among them. They were unaware of their rights and believed that their husbands should make the decisions. The study also found that infertility is still considered a woman’s problem and that she must face the stigma and violence associated with it. Indigenous women also believe that abortion is a sin and that they should not resort to it, even when there is a medical emergency. Navya, who ignored the doctor’s advice on abortion, went through the physical and mental trauma of pregnancy, followed by the child’s death. However, she believed that she had made the right decision. The prevalence of myths and misconceptions, in relation to matters such as sexuality, contraception, infertility, and abortion, immensely affects choices and decisions related to sexual and reproductive behaviors. Furthermore, inadequate SRHR information, decision-making capacity, and access to quality SRH services complicate the reproductive health status of indigenous women, leading to higher maternal and infant mortality rates.
Gender bias and discrimination are embedded in women’s cultural beliefs and traditional practices. Case studies have revealed that patriarchal notions and power relations control the willingness and abilities of women, depriving them of realizing their sexual and reproductive health rights. The experiences of indigenous women indicate unequal knowledge, opportunities, and access to sexual and contraceptive information as compared to their husbands. Consequently, women lack the autonomy to decide on matters such as contraception choices and decisions regarding the number of children. Furthermore, culturally insensitive healthcare services intensify indigenous women’s vulnerabilities. These tendencies perpetuate women’s inferior position and hamper the attainment of practical and strategic gender needs. Access to education, including comprehensive sexuality education, and to sexual and reproductive health services is essential in supporting the autonomy and agency of women and girls (Lundius, 2019).
The intergenerational comparison found a slightly positive change among younger compared with older generations. Social networking platforms and the health interventions of field-level workers may have led to such changes. However, the unequal relations between partners, the prevalence of gender norms embedded in cultural practices and traditional beliefs, and lack of access to resources intersect, creating barriers to the fulfilment of the sexual and reproductive health rights of indigenous women.
Conclusion
This intergenerational study based on dyadic interviews reveals that the sexual and reproductive health experiences of indigenous women in Attappady are shaped by certain myths and misconceptions and that beliefs about impurities and the alienation of women’s bodies still exist among indigenous communities. The fear of social exclusion, an unhealthy diet, uninformed choices, and the stigma and trauma related to sexual and reproductive health events negatively impact indigenous women’s physical and mental health. Furthermore, lack of access to quality healthcare services, lack of male engagement, and lack of decision-making capacity result in the denial of rights.
In conclusion, intergenerational changes are minimal among indigenous women and the existence of gender-power relations has been identified, which is critical in determining the perpetuation of myths and misconceptions regarding sexual and reproductive health experiences. The findings of this study emphasize the need for culturally sensitive community interventions from an intersectional perspective aimed at eliminating myths and misconceptions and generating awareness of sexual and reproductive health rights among indigenous women.
Acknowledgments
This paper is based on the first author’s doctoral work on the reproductive health experiences of indigenous women from an intergenerational analysis in Attappady performed under the guidance of the second author.
References
-
Anderson, I., Robson, B., Connolly, M., Al-Yaman, F., Bjertness, E., King, A., …&Yap, L. (2016). Indigenous and tribal peoples’ health (The Lancet – Lowitja Institute Global Collaboration): a population study. The Lancet, 388(10040), 131–157.
[https://doi.org/10.1016/S0140-6736(16)00345-7]

-
Adongo, P. B., Tabong, P. T. N., Azongo, T. B., Phillips, J. F., Sheff, M. C., Stone, A. E., & Tapsoba, P. (2014). A comparative qualitative study of misconceptions associated with contraceptive use in southern and northern Ghana. Frontiers in Public Health, 2, 137.
[https://doi.org/10.3389/fpubh.2014.00137]

-
Asmat, S., Manhas, S., Sharma, A., Fatima, N., & Hassan, N. (2020). Socio-cultural belief and practices related to menarche and menstruation among tribals of Kargil, Jammu and Kashmir. Journal of Krishi Vigyan 2020, 8(2), 271–278.
[https://doi.org/10.5958/2349-4433.2020.00055.0]

-
Bandyopadhyay, M. (2009). Impact of ritual pollution on lactation and breastfeeding practices in rural West Bengal, India. International Breastfeeding Journal, 4(2), 1–8.
[https://doi.org/10.1186/1746-4358-4-2]

-
Begum, S., Sebastian, A., Kulkarni, R., Singh, S., & Donta, B. (2017). Traditional practices during pregnancy and childbirth among tribal women from Maharashtra: A review. International Journal of Community Medicine and Public Health, 4(4), 882–885.
[https://doi.org/10.18203/2394-6040.ijcmph20171301]

- Bell, L. (2014). Ethics and feminist research. In S. N. Hesse-Biber (Ed.), Feminist research practice - A primer (pp. 73–106). London: Sage.
-
Carastathis, A. (2014). The concept of intersectionality in feminist theory. Philosophy Compass, 9(5), 304–314.
[https://doi.org/10.1111/phc3.12129]

- Deogaonkar, S. G. (1990). The hurdles in tribal development. In R. S. Negi & J. S. Gaikwad (Eds.), A sociocultural dynamics of tribal development (pp. 1–5). Pune, Maharashtra: Tribal Research Institute.
-
Dhingra, R., Kumar, A., & Kour, M. (2009). Knowledge and practices related to menstruation among tribal (Gujjar) adolescent girls. Studies on Ethno-Medicine, 3(1), 43–48.
[https://doi.org/10.1080/09735070.2009.11886336]

- Galati, A. J. (2015). Onward to 2030: Sexual and reproductive health and rights in the context of the sustainable development goals. Guttmacher Policy Review, 18(4), 77–84.
- Hansdah, R., & Rath, A. (2021). Traditional practices and belief in prenatal and postnatal care of tribal women: A study from the tribal area of Jajpur district. Journal of Emerging Technologies and Innovative Research (JETIR), 8(6), 865–869.
- Haraway, D. (1988). Situated knowledges: The science question in feminism and the privilege of partial perspective. Feminist Studies, 14(3), 575–599.
- International Institute for Population Sciences (IIPS) and ICF (2021). National Family Health Survey (NFHS -5), 2019-21. Retrieved March 23, 2023, from https://dhsprogram.com/pubs/pdf/FR375/FR375.pdf
- Kaur, T. P. (2019). Integrating age old cultural reproductive health practices with modern medicine to bring down morbidity and mortality among Birhor tribes of Jharkhand, India. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 8(1), 25.
- Lundius, J. (2019, February 4). Sex education and women’s health. Inter Press Service. Retrieved March 23, 2023, from http://www.ipsnews.net/2019/02/sex-education-womens-health
- Manikandan, A. D. (2014). A tragedy unfolding: tribal children dying in Attappady. Economic and Political Weekly, 49(2), 1–7.
-
McCall, L. (2005). The complexity of intersectionality. Signs: Journal of Women in Culture and Society, 30(3), 1771–1800.
[https://doi.org/10.1086/426800]

- Ministry of Health and Family Welfare. (2018). Tribal health in India bridging the gap and a roadmap for future. Retrieved March 23, 2023, from https://nhm.gov.in/New_Updates_2018/NHM_Components/Health_System_Stregthening/tribal_health/Tribal-Health-Report.pdf
- Murshid, V., & Krishnaprabha V. (2018). Nutritional status and birth outcome of Mudukas tribal pregnant women in Attapady block, Kerela. International Journal of Science and Research, 7(5), 1257–1259. https://www.ijsr.net/getabstract.php?paperid=ART20182806
- Nair, M. S., & Saisree K. G. (2021). Impact of tribal development programmes: Analysis based on Attappady tribal development block, Kerala. International Journal of Humanities and Social Science Invention, 10(5), 17–23. https://www.ijhssi.org/papers/vol10(5)/Ser-2/D1005021723.pdf
- Nazir, T. (2022, May 6). Kerala govt launches initiative to improve health of tribal women, plug infant deaths. Retrieved March 23, 2023, from https://thelogicalindian.com/health/kerala-govt-launches-initiative-to-improve-health-of-tribal-women-35399
- Office of the Registrar General & Census Commissioner, India. (2011). Primary census abstract data for scheduled tribes (ST) (India & States/ UTs—District Level). Retrieved September 29, 2022, from ww.censusindia.gov.in/2011census/populationenumeration.html, .
-
Palo, S. K., Samal, M., Behera, J., & Pati, S. (2020). Tribal eligible couple and care providers’ perspective on family planning: A qualitative study in Keonjhar district, Odisha, India. Clinical Epidemiology and Global Health, 8(1), 60–65.
[https://doi.org/10.1016/j.cegh.2019.04.008]

- Pariyaram Medical College. (2016). Report on health status of Tribal in Attapadi. Retrieved March 23, 2023, from https://www.researchgate.net/publication/289868263_Report_on_health_status_of_Tribal_in_Attapadi
- Rajitha K. V. P., & Kuruvilla, M. (2021). Unexplored gender dimensions of ritual practices: Study on tribal communities in Wayanad, Kerala. Online International Interdisciplinary Research Journal, 11(August), 157–164.
-
Sengupta, A. (2019). Maternal health in underserved tribal India. Sexual and Reproductive Health Matters, 27(1), 304–306.
[https://doi.org/10.1080/26410397.2019.1581534]

- Srivastava, R., & Sahu, D. R. (2022). Understanding cultural sensitivity and competence in health care: Reflections on antenatal care from rural Lucknow. Explorations, E-Journal of the Indian Sociological Society, 6(1), 130–146.
-
Starrs, A. M., Ezeh, A. C., Barker, G., Basu, A., Bertrand, J. T., Blum, R., … & Ashford, L. S. (2018). Accelerate progress—sexual and reproductive health and rights for all: Report of the Guttmacher–Lancet Commission. The Lancet 391(10140), 2642–2692.
[https://doi.org/10.1016/S0140-6736(18)30293-9]

-
Thipanyane, M.P., Nomatshila, S.C., Oladimeji, O., & Musarurwa, H. (2022). Perceptions of pregnant women on traditional health practices in a rural setting in South Africa. International Journal of Environmental Research and Public Health, 19(7), 4189.
[https://doi.org/10.3390/ijerph19074189]

- United Nations. (2015). Sustainable development goals. Retrieved September 29, 2022, from https://www.un.org/sustainabledevelopment/sustainable-development-goals/
- UN Office of the High Commissioner for Human Rights. Sexual and reproductive health and rights. (n.d). Retrieved March 23, 2023, from https:/www.ohchr.org/en/women/sexual-and-reproductive-health-and-rights
- Women’s Health Research Network. (2009). Intersectionality: Moving women’s health research and policy forward. Retrieved March 23, 2023, from https://www.researchgate.net/publication/238733273_Intersectionality_Moving_Women's_Health_Research_Policy_Forward
Biographical Note: Asha Sankar V. is a Ph.D. scholar at the Department of Women’s Studies, University of Calicut, Kerala, India. She gained a Master’s Degree in Social Work from Vimala College, University of Calicut and then worked with the Tata Institute of Social Sciences Kerala Centre as Research Assistant. Her areas of interest include gender and health, marginalized social groups, livelihoods, poverty, and development.
Biographical Note: Dr. Moly Kuruvilla is a Professor of Women’s Studies at the Department of Women’s Studies, University of Calicut, Kerala, India. She is the co-editor of the Handbook of Research on New Dimensions of Gender Mainstreaming and Women Empowerment published by IGI Global, California, in June 2020, and Gendered Experiences of COVID-19 in India published by Palgrave Macmillan in November 2021. She is an advisor to the Asian African Association for Women, Gender and Sexuality.